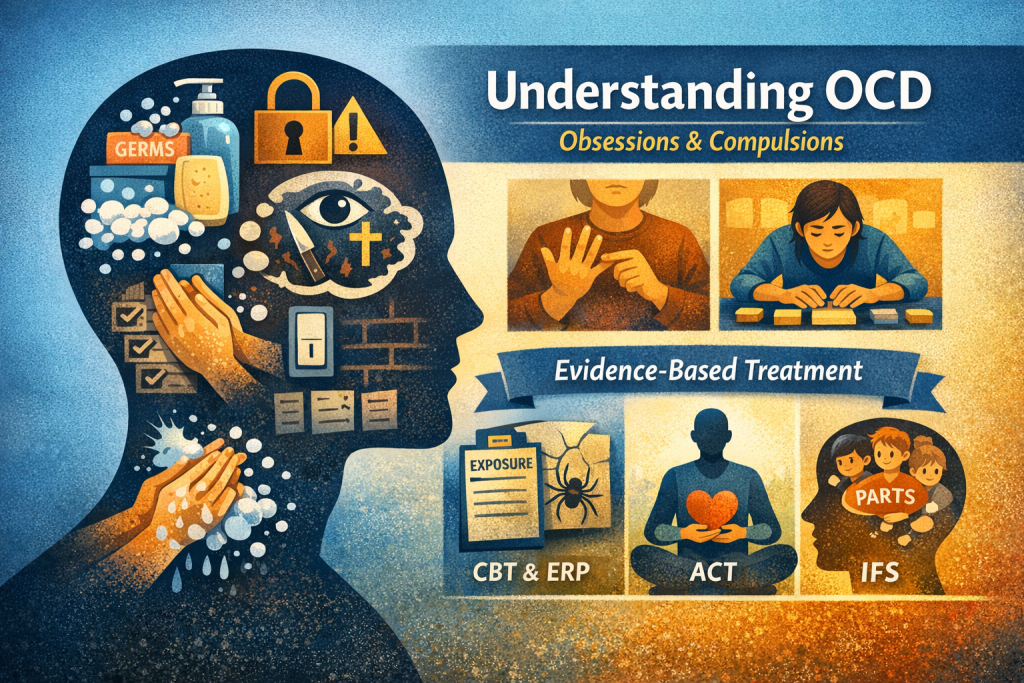
Understanding OCD: Types, Symptoms & Evidence-Based Treatment
Learn how to recognize different forms of obsessive-compulsive disorder (OCD), distinguish compulsions from strong preferences or common worries, and explore how evidence-based therapies—like CBT with Exposure and Response Prevention (ERP), ACT, and IFS—help people recover.
What Is OCD?
Obsessive-compulsive disorder (OCD) is a mental health condition marked by obsessions (repeated, intrusive thoughts, urges, or images) and compulsions (repetitive behaviours or mental acts performed to reduce distress or prevent feared outcomes). If untreated, OCD can significantly interfere with daily life, relationships, and functioning.
Different Types of OCD
While every person’s experience with OCD is unique, common subtypes include:
1. Contamination / Cleaning OCD:
Fear of germs, illness, dirt or contamination. Compulsions often involve washing or cleaning.
2. Checking OCD:
Worries about harm, safety or mistakes lead to compulsions like repeatedly checking locks, stoves, or appliances.
3. Symmetry / “Just Right” OCD:
A need for things to feel perfect, orderly or symmetrical; compulsions involve arranging or repeating actions until it feels right.
4. Intrusive Thought / Pure-O:
Distressing thoughts (e.g., violent, sexual, blasphemous themes) with mental rituals like rumination or silent checking.
5. Hoarding-Related OCD:
Difficulty discarding items due to anxiety about needing them or fear of harm if discarded.
Each subtype reflects a pattern of obsessions (thoughts/feelings) and compulsions (actions/mental rituals) that drive behaviour. People can experience multiple subtypes at once.
Obsessions vs. Worries & Thoughts
Many people worry or have unwanted thoughts — that’s human. With OCD:
• Obsessions are intrusive, recurrent, distressing, and often feel uncontrollable. They don’t just go away with distraction.
• Common worries are typically proportionate to life stressors and don’t demand repeated mental or behavioural responses.
Key differences:
• Frequency and intensity: OCD obsessions recur often and provoke significant anxiety.
• Relevance to real life: Everyday worries tend to be grounded in current events and are resolved as life circumstances change.
• Impact on functioning: OCD obsessions interfere with work, school or relationships; routine worries usually don’t.
Compulsions vs. Strong Preferences
It’s natural to like routines or order. But:
Compulsions in OCD are:
• Driven by intense anxiety or fear of harm.
• Performed to neutralise distress (e.g., checking repeatedly to avoid disaster).
• Time-consuming and hard to resist.
Strong preferences are:
• Behaviour choices based on comfort or habit, not anxiety relief.
• Flexible (can postpone or adapt without distress).
If skipping a behaviour causes intense distress or fear of something bad happening — that’s more consistent with how a compulsion is experienced.
Evidence-Based Treatment for OCD
Research shows that targeted psychological therapies can significantly reduce OCD symptoms when applied correctly and consistently.
Cognitive Behavioural Therapy (CBT)
CBT is a structured, goal-oriented therapy that helps people understand the link between thoughts, feelings, and behaviours. For OCD, CBT typically involves:
• Exposure and Response Prevention (ERP):
This is the cornerstone of CBT for OCD, where the person gradually confronts feared thoughts or situations without performing compulsive rituals. Over time, this reduces anxiety and weakens the obsession-compulsion cycle. ERP is backed by strong clinical trial evidence as an effective treatment for diverse OCD presentations.
• Cognitive strategies:
These help identify and reframe unhelpful beliefs (e.g., overestimating responsibility, intolerance of uncertainty), making it easier to stick with exposures. Integrating cognitive work can improve engagement and outcomes.
Together, CBT with ERP is widely recognized as the first-line psychological treatment for OCD.
Acceptance and Commitment Therapy (ACT)
ACT focuses on:
• Accepting uncomfortable thoughts and feelings rather than fighting or avoiding them.
• Identifying personal values and committing to actions aligned with those values.
ACT helps people relate differently to obsessions — seeing them as mental events rather than threats that must be neutralised — which can reduce the need to engage in compulsions. ACT can be especially helpful when ERP is initially too challenging or for residual symptoms after CBT/ERP.
IFS is a therapeutic approach that views the mind as composed of “parts” with different roles (e.g., a part that worries and a part that protects). In OCD, certain parts may push compulsions to reduce anxiety. IFS helps:
• Understand the internal roles of these parts.
• Build compassionate self-leadership.
• Reduce conflict between parts that drive obsessions and those resisting treatment.
While IFS is not a first-line treatment like CBT/ERP, it can be a supportive adjunct when integrated into a broader treatment plan.
How We Help With OCD
In our clinical psychology approach, helping someone with OCD starts with a thoughtful and collaborative assessment:
- Explore your unique experience – We identify your specific obsessions and compulsions using structured interviews and proven assessment tools.
- Understand what’s driving the behaviour – We distinguish OCD from strong preferences or everyday worries by looking at how much distress it causes, how it affects your daily life, and what function the behaviour serves.
- Build a personalized treatment plan – Based on your needs and preferences and previous therapy experiences, we combine evidence‑based strategies such as:
- ERP exercises: Gradual, guided exposure to feared situations or thoughts.
- Cognitive work: Addressing unhelpful beliefs and patterns.
- ACT or IFS elements: When helpful, we focus on acceptance, values, and understanding the different “parts” of yourself to support inner balance.
- Track progress and adjust as we go – We regularly check in to see what’s working, making the plan practical, flexible, and sustainable.
Finding An Easier Way Forward
OCD is a complex but treatable condition. Understanding the types of OCD, knowing how obsessions and compulsions differ from everyday thoughts and preferences, and using therapies grounded in evidence — especially CBT with ERP — increases the likelihood of meaningful improvement. ACT and IFS can complement core CBT work, offering flexibility and deeper emotional insight.
If you’re exploring treatment for yourself or someone you care about, a mental health professional trained in OCD-specific therapies can guide a safe, effective plan based on current research and clinical best practices. We invite you to contact us.
References:
Reid JE, Laws KR, Drummond L, Vismara M, Grancini B, Mpavaenda D, Fineberg NA. Cognitive behavioural therapy with exposure and response prevention in the treatment of obsessive-compulsive disorder: A systematic review and meta-analysis of randomised controlled trials. Compr Psychiatry. 2021 Apr;106:152223