Cognitive Behaviour Therapy (CBT)
CBT was developed in the 1960s to help treat mood and anxiety symptoms. CBT is a structured treatment that focuses on the role of thoughts and behaviour on psychological and emotional problems such as depression and anxiety, and many other concerns such as trauma or PTSD, OCD, addictions, eating disorders and insomnia.
Because it has been around for many decades, CBT is often more commonly known and recommended by doctors, insurers and other professionals.
CBT is not necessarily more effective than other treatments such as ACT. In fact, research often concludes that other approaches are just as effective as CBT. However, there tends to be more studies on CBT because this therapy modality has been around the longest, and its structure lends itself well to controlled research and group formats.
In particular, CBT is a therapy that is often delivered in a ‘manualized’ format, where a specific number of sessions is prescribed and the content and delivery of those sessions may be pre-determined. This is often preferred in hospital or community health settings because of the cost and lostical advantages of delivering therapy in a group format.
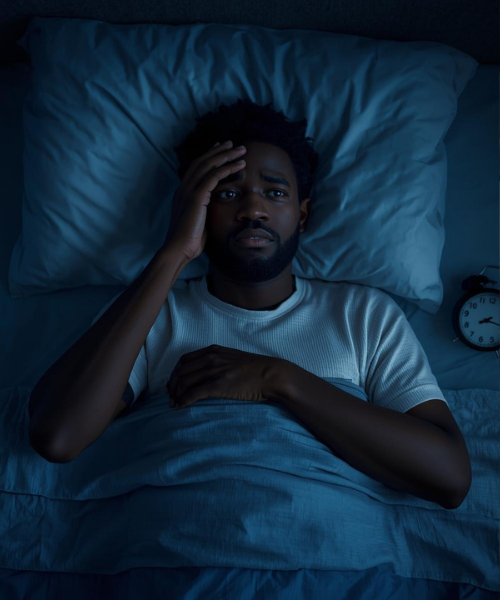
CBT can be very effective for a wide range of concerns such as depression, anxiety, OCD, trauma, eating disorders, alcohol and addiction issues and anger problems as long as patients or clients actively participate in the treatment and complete homework or between-session work.
CBT interventions focus on helping individuals to become aware of and shift or challenge the content of their negative thinking. Our style of thinking (e.g., when we generalize, catastrophize or discount the positives etc) is known to significantly impact on our mood, feelings and behaviour. An example of an intervention commonly used in CBT is ‘thought monitoring’, where people are taught to notice and monitor negative thinking styles (at first using a thought record) in order to label their thoughts and then challenge their thoughts with socratic dialogue and/or specific questions.
CBT interventions also focus on behaviour. Behaviour has a significant impact on mood and feelings. By changing our behaviour we can start to change the way we feel and think. For example, behavioural activation is a common intervention used for depression where people are taught structured ways to increase meaningful mastery and leisure tasks in order to improve mood. Another important CBT behavioural intervention is exposure therapy, which is commonly used to help treat anxiety symptoms, including:
triggers in PTSD, and
Exposure and response prevention for OCD symptoms.
References:
Samaen, M., et al., (2020). A clinical effectiveness trial comparing ACT and CBT for inpatients with depressive and mixed mental disorders.
Website resources:
Centre for Clinical Interventions : free structured CBT workbooks.